DISC DEGENERATION: WHAT'S NORMAL?
The Cause | MRI Appearance| Pathological Aging/Degeneration |
On the following two pages, we will study the two types of disc degeneration: natural disc degeneration, which we will talk about first, and then the pathological type, which can be the "ground floor" for the major causes of the disc -related back and leg pain.
Natural Disc Aging:
 Unlike other tissues of the human body, the poorly vascularized intervertebral disc tends to undergo degeneration of its internal structure at a surprisingly early age. In fact, award-winning research has demonstrated such degeneration usually begins within the first decade of life! (6,15)
Unlike other tissues of the human body, the poorly vascularized intervertebral disc tends to undergo degeneration of its internal structure at a surprisingly early age. In fact, award-winning research has demonstrated such degeneration usually begins within the first decade of life! (6,15)
Thankfully, most of the time this degeneration is harmless and considered just part of the natural aging process. However, in some people, this degeneration process can run amok and result in severe chronic and disabling back pain. [8,14,151,152]
Why some people's discs succumb to such severe pathological disc failure (above right) and others don't continues to be a mystery, although heredity certainly plays a significant role in this process.
It is this abnormal accelerated/pathological form of disc aging and degeneration which is called Degenerative Disc Disease (DDD).
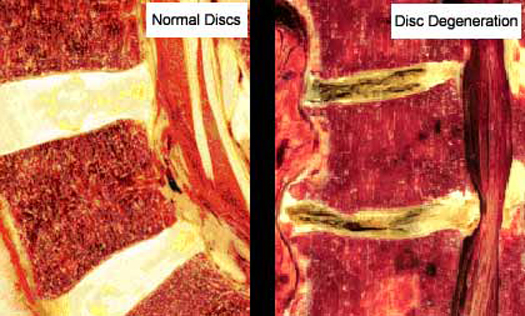
The figure above demonstrates cadaver examples of a normal looking disc (left) versus discs that have undergone severe pathological degeneration (i.e., advanced DDD).
What's the Cause?
It is believed that natural disc aging occurs secondary to the horrible environment that cells of the nucleus and annulus are exposed to. Specifically, only the outer periphery of the disc has blood vessels which can supply these outer annular cells with oxygen and nutrients and easily remove their waste products. The rest of the disc, however, does not have a direct blood supply! Therefore, these disc cells must get their oxygen, nutrients, and waste removal from blood that is within the the subchondral bone of the vertebral body! In other words, they have no direct blood supply, which is a rarity in the human body!
Specifically, blood must "diffuse" into the substance of the disc through tiny holes within the subchondral bone. Therefore, even in a "normal" disc, the feeding/waste removal system is terrible and makes it tough for self to stay alive.
With the passage of time, these tiny holes start to close which in turn makes the environment of the disc even worse than it is to begin with. Slowly but surely disc cells start to die, and as they die the disc becomes dehydrated and brittle. [700, 5]
Therefore, any attempts at injecting new disc material into a degenerated disc (such as live disc cells)--in hope of healing the damaged disc--will only lead to failure, for the new disc material will soon meet the same fate of the original disc tissue: it will starve to death.
Although we will discuss pathological disc aging in the next page, there is no doubt that if the normal disc degeneration process gets sped up by any condition, it can result in disabling low back pain secondary to annular tears, disc herniations, and even spinal stenosis. [201, 206, 219, 227]
What are my chances of getting DDD? According to the medical research, approximately 10% of the population will suffer DDD -related chronic back and/or chronic leg pain which results in permanent disability. [250-253, 203, 209, 216, 231, 900, 904, 905, 906, 227]
The MRI Appearance:
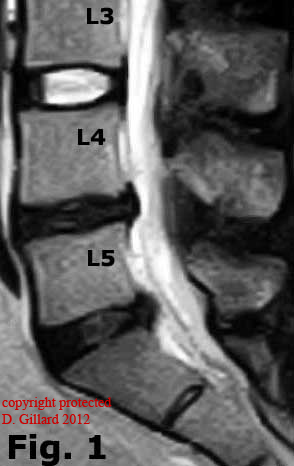 The diagnosis of DDD is best made on T2-weighted MRI imaging (Fig.#1) (27), although some of the late appearances of DDD (disc collapse, osteophytosis, and sclerosis) may also be seen on CT scan and X-ray. Such MRI appearances are easy to spot and are characterized by a loss of signal intensity (loss of whiteness or hypointense) of discal tissue, which makes the disc appear black instead of bright white. Technically, this blackening of the disc(s) occurs because the disc has dehydrated (lost water content) and is dying. This 'blackening' is called disc Desiccation. Since the MRI signal intensity (whiteness) is directly related the disc's water content (215,226), any loss of discal water will proportionally decrease the 'whiteness' of that disc on T2-weighted MRI. So, in layman's terms, the dryer the disc, the blacker and more degenerated it will look on MRI. Figure #1: Here is the classic presentation of DDD as seen in this T2-weighted sagittal (lateral) image. Note the bright white and healthy L3 disc (above the L4 vertebra) in comparison to the 'black' and desiccated L4 and L5 disc. Also note a 4mm herniation at the L4 disc (between L4 and L5 vertebrae) and a 9mm herniation at the L5 disc. Also note there is a loss of disc height at both L4 and L5, in comparison to the thicker L3 disc.
The diagnosis of DDD is best made on T2-weighted MRI imaging (Fig.#1) (27), although some of the late appearances of DDD (disc collapse, osteophytosis, and sclerosis) may also be seen on CT scan and X-ray. Such MRI appearances are easy to spot and are characterized by a loss of signal intensity (loss of whiteness or hypointense) of discal tissue, which makes the disc appear black instead of bright white. Technically, this blackening of the disc(s) occurs because the disc has dehydrated (lost water content) and is dying. This 'blackening' is called disc Desiccation. Since the MRI signal intensity (whiteness) is directly related the disc's water content (215,226), any loss of discal water will proportionally decrease the 'whiteness' of that disc on T2-weighted MRI. So, in layman's terms, the dryer the disc, the blacker and more degenerated it will look on MRI. Figure #1: Here is the classic presentation of DDD as seen in this T2-weighted sagittal (lateral) image. Note the bright white and healthy L3 disc (above the L4 vertebra) in comparison to the 'black' and desiccated L4 and L5 disc. Also note a 4mm herniation at the L4 disc (between L4 and L5 vertebrae) and a 9mm herniation at the L5 disc. Also note there is a loss of disc height at both L4 and L5, in comparison to the thicker L3 disc.
Why some discs prematurely degenerate (DDD) and cause chronic pain and others don't is still somewhat controversial, however, it is becoming clearer that poor genetics (397-399,403,413a); a past history of moderate to severe spinal trauma; or have an occupation that is heavy, and labor-intensive are the main risk factors (201,16). These factors will be discussed in depth below.
WARNING: WERE ABOUT TO GET TECHNICAL SO HANG ON!
NATURAL DISC AGING: (aka: NDA)
The most common and striking feature of disc aging and degeneration is the loss of the proteoglycan molecule from the nucleus of the disc (333, 26). Other findings of aging include a progressive dehydration (18), a progressive thickening (via cross-linking, glycation and CML formation), brown pigmentation formation (66) and increased 'brittleness' of the tissues of the disc (62).
The Two Main Factors of Disc Aging:
There are two main factors that are involved in the aging process of the disc and both of these factors are amplified because of the already poor vascular supply of the disc:
1) Idiopathic blood vessel/nutrient loss and dehydration:
The short version: For unknown reasons the nucleus of the disc losses much of its vital blood supply during the first decade of life (6). Without sufficient nutrients (which are contained in the blood) the cells of the disc begin to die (500) and the disc (especially the nucleus) becomes depleted of water. The drop in water/proteoglycan content is one or the classic signs of disc aging (333). Because of this dehydration of the nucleus, there is ultimately a 'weight-bearing shift' that occurs from the nucleus onto the outer annulus, ring apophysis, and the zygapophyseal joints. This increase stress upon the preceding posterior structures may lead to further more severe forms of aging, i.e., DDD.
The long version: Under the physiology section of the 'Disc Anatomy' page, we have learned how important disc nutrition is in maintaining a normally functioning disc. To recap: as long as the cells of the disc receive an adequate nutrient supply (which is obtain from the diffusion of oxygen, glucose, and amino acids [pink balls] from capillary beds just above the end-plates, into the disc), they will happily manufacture the proteoglycan molecule, which combines within the disc to form the larger aggrecan and aggregate molecules. It is these aggrecan molecules that trap and hold water within the disc. A fully hydrated disc will have a very high hydrostatic pressure (osmotic pressure) which makes the nucleus pulposus (which is 80% water in a normal disc) incredibly strong and able support the lion's share of the axial load from the body.
 Remember, the nutrients in the inner annulus and nucleus have a 'crummy feeding system' to being with. As you can see on the model on the left, the nutrients (pink balls) have a long way to 'diffuse' in order to reach all the disc cells.
Remember, the nutrients in the inner annulus and nucleus have a 'crummy feeding system' to being with. As you can see on the model on the left, the nutrients (pink balls) have a long way to 'diffuse' in order to reach all the disc cells.
Without an adequate supply of nutrients, the cells of the disc will die. The preceding fact was substantiated by the 2001 Volvo Award winning study of Horner and Urban (500), who studied the viability of living human disc cells under different conditions. They concluded that if the cells of the disc failed to get proper nutrients - such as oxygen, or glucose - or if the pH level of the disc rose (because waste is not being diffused out of the disc), disc cells would die and stop producing the vital proteoglycan molecule; without proteoglycans, the disc losses its water content (dehydrates) and losses its hydrostatic pressure (osmotic pressure) (241). This lost proteoglycan content is the most striking feature of disc aging and degeneration (333). Other research has confirmed this cell death as well. In 1982, Trout and Buckwalter discovered that by adulthood over 50% of the cells of the disc were dead (321).
So what's killing the disc cells and resulting in this loss of proteoglycan content?
Starvation! It seems that the human disc becomes 'nutritionally compromised' from the moment we begin to stand and walk. In 2002, Boos et al. observed an idiopathic "obliteration" of portions of the nutrient-providing capillary beds, which lie just above the vertebral end-plates. (Remember that these capillary beds are the ONLY source of nutrients for the cells of the inner annulus and nucleus.) Amazingly, this 'auto-destruction' begins within the first two years of life, and worsens over the next 8 years. Specifically, they stated that between the ages of 3 and 10 there was "a dramatic decrease of physiologic vessels in the end-plate..and an abundance of areas with obliterated vessels. and a substantial increase in (disc) cell death." (6) THESE FINDINGS WERE THE 'SMOKING GUN' that scientists had been waiting for and suggested that the initial causation of disc aging and degeneration was 'nutritional compromise', secondary to an idiopathic loss of the discal blood supply above the vertebral end-plates. Needless to say, Boos and company won the '2002 Volvo Award in Basic Science' for this most shocking discovery.
Other factors affecting disc nutrition via diffusion rates of nutrients through the vertebral end-plates include end-plate calcification (506, 537, 538, 552,), the effects of changes in blood flow patterns secondary to arterial stenosis (522, 524-527), smoking, diabetes, and exposure to vibration (500, 517).
The Vicious Cycle of Disc Aging:
This progressive loss of proteoglycan and dehydration begins to 'snowball' out of control. Not only because of the progressive loss of nutrients, but also because of the fact that decreased hydrostatic pressure also slows the production of proteoglycan by the disc cell (11). Here's what this vicious cycle looks like:
As the nutrient supply within the disc drops (because of blood vessel obliteration and later end-plate mineralization), the disc cells start to die. Because there are fewer available disc cells around to make proteoglycan, there is a drop in the amount of circulating proteoglycan aggrecan molecules. This decrease in the aggrecan molecule, (which is what holds water within the disc) results in both dehydration, and a decrease in hydrostatic pressure within the nucleus. The loss of hydrostatic pressure has two negative effects on the disc: a) it will cause a further decrease in the amount of circulating proteoglycan aggrecan molecules, for we know from the work of Handa et al. that disc cells need a constant hydrostatic pressure level of 3 atm to function normally (11). Any increase or decrease in hydrostatic pressure caused a reduction proteoglycan production, which in turn decreases hydrostatic pressure even more - hence the vicious cycle. b) Now, these biochemical changes begin to change the biomechanics of the disc: With the decrease of hydrostatic pressure the nucleus, like a deflating beach-ball, can no longer carry the full axial-load (weight) of the body. A 'shift' in the axial-load distribution begins to occur, with the periphery of the disc (outer anulus, ring apophysis, and zygapophyseal joints) taking on more and more of the load and stress. Experimentally, the anulus of a degenerated disc shows a very high 'stress-load' on the anulus and NOT the nucleus (17 ,12 ). We will later learn that this 'load-shift' can be greatly accelerated if the volume of the nucleus is increased by trauma-induced structural damage to either the end-plate (compression fracture) and/or tearing of the inner anulus.
2.) Non-Enzymatic Glycation & the aging process: Glycosylation (aka: Glycation)
Glycation (aka: Glycosylation , or non-enzymatic glycation) is a biochemical reaction which occurs when reduced sugars (like glucose) come in contact with proteins (like disc collagen) in an avascular relatively-anaerobic environment. The more avascular the tissue, the more severe this reaction occurs. Since the disc is the largest avascular tissue in the body, the glycation process thrives within its substance and results in a slow but steady transformation of disc collagen into a thicker but more brittle substance. Specifically, this reaction occurs between the protein molecules within the collagen, and free floating glucose (reduced sugar). This reaction is called 'posttranslational protein modification' or simple Glycation. Here's how it works: In the absents of oxygen, reduced sugars start to 'rub against' (bind) the proteins within the collagen. The proteins can only take so much 'rubbing', and soon are transformed into what is called an 'Advanced Glycation End-Product' or AGE. These converted discal collagen strands (AGEs) become much more brittle and also much more 'sticky', i.e., they love to combine with their glycated neighbors in a process called 'cross-linking'. This 'cross-linking' phenomenon makes the disc thicker, more fibrous and more susceptible to the development of DDD (62). It also stains the discal tissue a distinct shade of brown (66) as noted in figure #2.
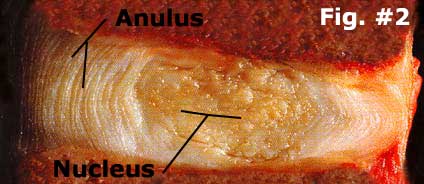 Fig. #2: Here we have an example of early disc aging where the tissue of the human disc has turned somewhat brown in color compared to a healthy teen disc.
Fig. #2: Here we have an example of early disc aging where the tissue of the human disc has turned somewhat brown in color compared to a healthy teen disc.
It is important to understand, however, that this is a normal part of aging and is not considered pathological.
Again, the color change noted in figure 2 is the direct result of the glycation process described above. For comparison sake, let's take a look at a healthy teenage disc.
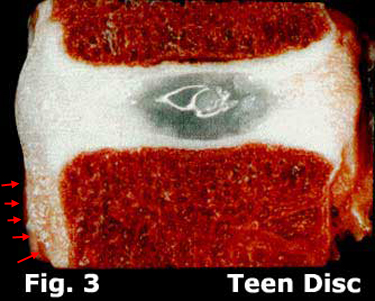 Figure 3 is a healthy human teenage disc which is completely void of visible glycolytic change.
Figure 3 is a healthy human teenage disc which is completely void of visible glycolytic change.
Note the bright white annulus fibrosus, which is completely surrounding the nucleus pulposus which is glistening because of its very high water content.
The vertebral endplates are also bright white and really not distinguishable in this image.
Also noteworthy is the disc herniation that has occurred in the posterior region, which has worked its way downward against the vertebra below (red arrows).
Finally, the unstable AGEs molecules, which produce another evil biochemical called the 'free radical', oxidize into a much more stable structure called a CML (N- Carboxymethyl -lysine). CML formation has been found to be an excellent indication of discal aging (15). In fact Andreas and Boos won the 1997 Volvo Award for their work in using the presents of CML-modified discal protein as an indicator for the various stages of aging (15). I'm not going to review this study for it's out of our scope, but for those of you who need-to-know, his paper is an excellent read.
Well, that about does it for the natural aging process of the disc. Let's now take a look at the more serious form of aging, DDD.
CURRENT RESEARCH:
700.) Benneker, et al. "2004 Young Investigator Award Winner: Vertebral Marrow Endplate Marrow Contact Channel Occlusion and Intervertebral Disc Degeneration." Spine. 2005; 30(2):167
5) Horner HA, Urban JPG, "Effects of Nutrient Supply on the Viability of Cells from the Nucleus Pulposus of the Intervertebral Disc: 2001 Volvo Award in Basic Science." Spine 2001; 26(23):2543-2549
Page 2 - Degenerative Disc Disease (DDD) | Reference Page | Top | Home
